Corneal transplants are surgical procedures that replace a damaged or diseased cornea with a healthy one from a donor. This procedure is necessary for people who have suffered from conditions such as corneal scarring, corneal swelling, or corneal degeneration, which can cause blurred vision, sensitivity to light, and even blindness. A corneal transplant can restore vision and improve the overall health of the eye. The success rate for corneal transplants is high, and with proper care and management, patients can enjoy improved vision for many years after the procedure.
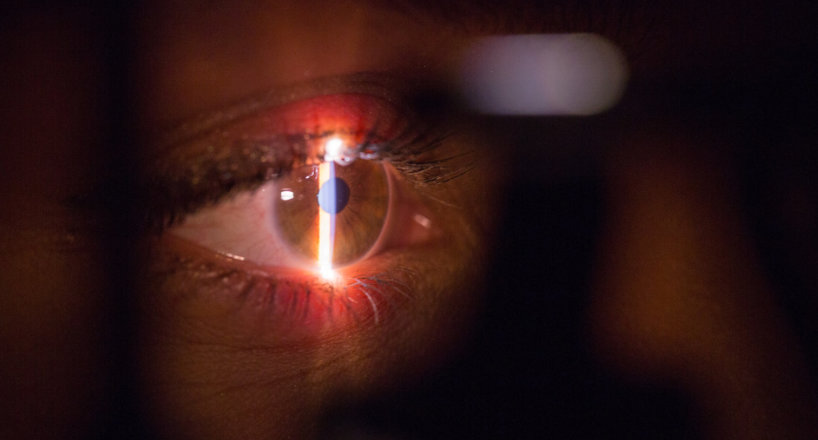
The cornea is the clear, front surface area of your eye. When a corneal transplant is done, officially termed keratoplasty (KP), the central part of the cornea is surgically gotten rid of and replaced with a “button” of clear and healthy corneal tissue contributed from an eye bank.
According to the National Eye Institute, roughly 40,000 corneal transplants are performed annually in the United States. The total success rate for keratoplasty is fairly high, yet up to 20% of clients may reject their donor corneas. Aggressive medical treatment with steroids is usually given up in response to indications of rejection, and it is frequently reliable at suppressing the negative reaction and conserving the cornea. At 5 to ten years after KP surgical treatment, studies report a motivating success rate of 95% to 99%.
Why are corneal transplants done?
Corneal transplants are typically done when the cornea ends up being broken or scarred in a manner that uncorrectable vision issues occur.
These types of vision conditions are not dealt with by glasses, contact lenses, or refractive laser surgical treatment (such as LASIK). Illness or injury is the normal culprit for vision loss.
Keratoconus is a typical factor for needing a corneal transplant. In this degenerative condition, the cornea thins and bulges forward in an irregular cone shape. Rigid gas permeable (GP) contact lenses can deal with mild cases by flattening the cornea, yet contacts are not effective when it concerns advanced stages of keratoconus. The National Keratoconus Foundation reports that 20% to 25% of individuals with keratoconus will need corneal transplant surgical treatment to bring back vision. Other corneal degenerative conditions will also lead to a need for keratoplasty.
Corneal ectasia is a thinning and bulging of the cornea that often happens after LASIK or other refractive vision correction treatments. On the occasion that this happens, a corneal transplant may be required to bring back vision.
Corneal scarring, due to chemical burns, infections, and other causes, is an additional reason that a corneal transplant may be suggested. Distressing injuries to the eye are likewise frequently responsible.

Corneal Transplant Procedure
Keratoplasty is typically done on an outpatient basis, without any requirement for overnight hospitalization. Relying on age, health condition and client choice, local or basic anesthesia is used.
Using a laser or a trephine, which is an instrument comparable to a cookie cutter, the surgeon cuts and gets rid of a round area of damaged corneal tissue and after that replaces it with the clear donor tissue.
Extremely great stitches are utilized to attach the donor button to the remaining cornea. The stitches stay in place for months (sometimes years) up until the eye has actually recovered, recovered totally, and is stable.
Healing from a Corneal Transplant
The overall healing time from keratoplasty might last as much as a year or longer.
Initially, vision will be blurred and the site of the corneal transplant might be swollen. In contrast to the rest of the cornea, the transplanted portion may be slightly thicker. For a few months, eye drops are applied to promote recovery and motivate the body to accept the new corneal graft.
A shield or glasses must be worn constantly after surgical treatment in order to protect the recovery eye from any bumps. As vision improves, clients might gradually go back to typical everyday activities.
What happens to vision post-keratoplasty?
Some patients report obvious enhancement as soon as the day after surgery. Yet a good deal of astigmatism is common after a corneal transplant. A client’s prescription for vision correction tends to fluctuate for a couple of months after the surgical treatment, and significant vision modifications may continue for as much as a year.
Hard, gas-permeable contact lenses generally supply the sharpest vision after a corneal transplant.
This is due to a residual irregularity of the corneal surface. Even with stiff contact lenses, spectacles with polycarbonate lenses need to be worn in order to supply adequate defense for the eye.
When the stitches are removed and recovery is complete, a laser procedure such as LASIK might be possible and recommended. Refractive laser surgery can lower astigmatism and upgrade the quality of vision, in some cases to the point that no eyeglasses or contact lenses are needed.